Antimicrobial resistance (AMR) is becoming an increasingly urgent global health issue, threatening the effectiveness of medications designed to treat infections. According to a recent study published in The Lancet, the number of deaths caused by drug-resistant infections could increase by nearly 70% by 2050.
From 2025 to 2050, more than 39 million deaths may be directly attributable to AMR, making it one of the most pressing public health challenges of our time. AMR occurs when bacteria, fungi, or other pathogens evolve to withstand the medications intended to eliminate them.
The overuse and misuse of antibiotics in humans, animals, and agriculture contribute significantly to the development of drug-resistant strains. Without effective medications, common infections could become life-threatening once again. The World Health Organization (WHO) has already listed AMR as one of the top global health threats, requiring immediate action.
Understanding Antimicrobial Resistance
Antimicrobial resistance happens when pathogens adapt to evade the effects of medications. This resistance makes standard treatments ineffective, leading to prolonged illnesses, more severe infections, and higher mortality rates.
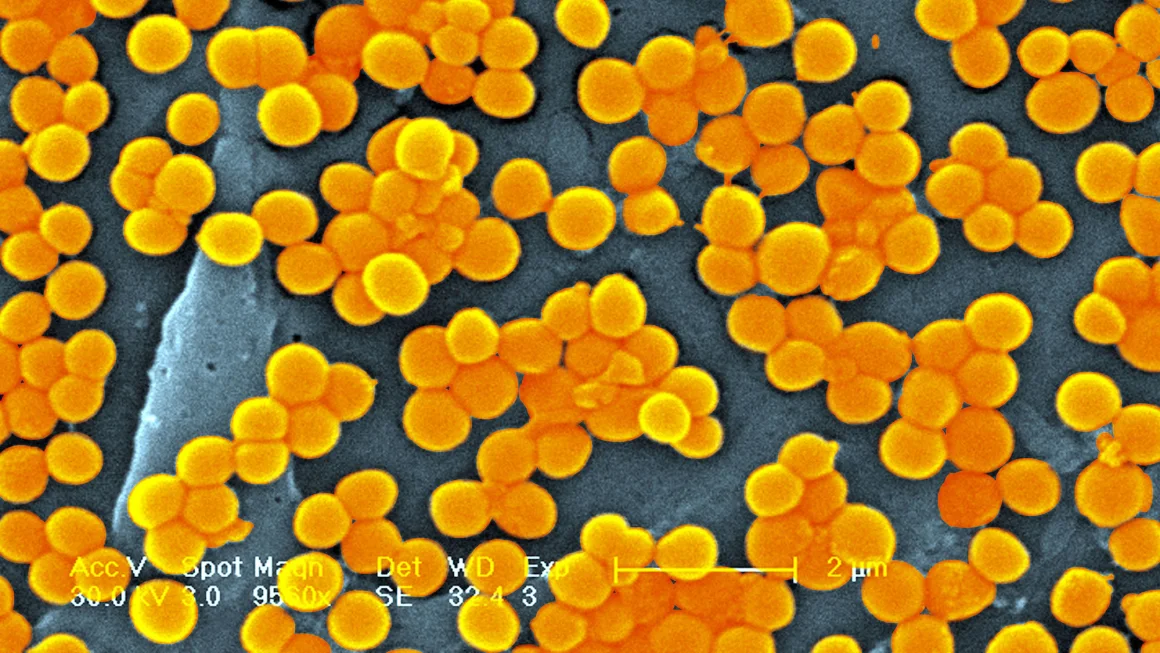
The improper use of antibiotics—whether in treating viral infections, unnecessary prescriptions, or overuse in farming—accelerates this process. Bacteria such as Staphylococcus aureus (including the methicillin-resistant MRSA strain) and Acinetobacter baumannii have evolved to resist even the most powerful drugs available.
These drug-resistant infections make it harder for healthcare providers to treat patients effectively, often requiring stronger medications with more severe side effects. In many cases, treatment options are dwindling, putting vulnerable populations, such as the elderly and those with underlying conditions, at particular risk.
Global Impact of AMR
The study published in The Lancet projects a significant rise in AMR-related deaths, particularly among older adults. Deaths from AMR-related infections have decreased among children under 5 due to improved sanitation, vaccines, and healthcare initiatives.
However, for adults aged 70 and older, deaths have surged by more than 80%. As the global population continues to age, these trends are expected to persist, making it essential to focus on older adults in AMR prevention efforts.
The research also found that regions such as South Asia, Latin America, the Caribbean, and sub-Saharan Africa are the hardest hit by antimicrobial resistance. In these areas, limited access to healthcare and medications further complicates the treatment of infections, leading to a higher death toll. In many low-resource settings, patients struggle to access even basic treatments like oxygen, which can be crucial for recovery from serious infections.
Why AMR is a Growing Concern

The rise of drug-resistant infections is alarming because it affects multiple areas of medicine. Procedures like surgeries, cancer treatments, and organ transplants rely on effective antibiotics to prevent infections.
Without these medications, routine medical procedures could become too dangerous to perform. Additionally, diseases like tuberculosis and pneumonia are becoming harder to treat, resulting in longer hospital stays, higher medical costs, and an increased risk of death.
Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most notorious drug-resistant pathogens, with deaths linked to MRSA infections nearly doubling from 1990 to 2021. This increase highlights how drug resistance makes once-treatable infections more deadly over time.
What Can Be Done to Combat AMR?
Addressing antimicrobial resistance requires a coordinated global effort. Public health experts have identified several strategies that can help mitigate the rise of drug-resistant infections:
-
Improving Antibiotic Stewardship
Proper use of antibiotics is essential. This includes prescribing antibiotics only when necessary and ensuring that patients complete their full course of treatment. Inappropriate use of antibiotics contributes to the development of resistant bacteria.
-
Investing in New Drug Development
The development of new antibiotics and alternative treatments is critical. Pharmaceutical companies and researchers must focus on creating medications that can target resistant pathogens effectively.
-
Better Access to Quality Healthcare
In low-resource settings, improving access to essential healthcare services, including medications, vaccinations, and clean water, is crucial. By preventing infections before they occur, fewer antibiotics will be needed, reducing the risk of resistance.
-
Reducing Antibiotic Use in Agriculture
Antibiotics are often used in livestock to promote growth and prevent disease. Reducing their use in agriculture can help slow the spread of resistant bacteria from animals to humans.
-
Raising Public Awareness
Educating the public on the dangers of antibiotic misuse is vital. People must understand that antibiotics are not effective against viruses like the common cold or flu and should be used only when prescribed by a healthcare provider.
New Treatment Approaches: A Ray of Hope
One promising solution to the growing superbug crisis is bacteriophage therapy. Bacteriophages, or phages, are viruses that target and kill specific bacteria. This therapy has been successful in treating patients with drug-resistant infections and offers an alternative to traditional antibiotics.
Phage therapy could also be used in conjunction with antibiotics to reduce the amount of medication needed and minimize the development of resistance.
Bacteriophages have shown effectiveness in cases where antibiotics failed, offering new hope in the fight against AMR. While more research and clinical trials are needed, phage therapy may become a vital tool in combating superbugs in the near future.
The Path Forward
The forecast for antimicrobial resistance is concerning, but it is not without hope. If countries work together to improve healthcare infrastructure, develop new treatments, and promote responsible antibiotic use, millions of lives could be saved. The study suggests that up to 92 million deaths could be prevented by 2050 if appropriate measures are taken, underscoring the importance of action today.
Reducing AMR requires a comprehensive approach that includes not only medical advancements but also policy changes and global cooperation. By focusing on prevention, responsible medication use, and innovative therapies like phage treatment, we can curb the rise of drug-resistant infections and protect future generations from the dangers of AMR.
Final Thoughts
The rise of antimicrobial resistance is one of the greatest public health challenges of our time, but with the right interventions, we can mitigate its impact. Continued research, investment in new medications, and global awareness are essential to ensuring that we have the tools to fight back against drug-resistant infections.
As we move forward, collaboration between healthcare providers, researchers, governments, and the public will be key in safeguarding the future of global health.